The life’s work of a Michigan surgeon demonstrates the importance of support for science research and big thinking.
1:00 PM
Author |
Hannah Cheriyan was born with her umbilical cord wrapped around her neck. Just hours old and in respiratory distress, she was airlifted to the Newborn Intensive Care Unit at University of Michigan C.S. Mott Children's Hospital.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
For four days, Cheriyan relied on a machine to perform the work of her heart and lungs, giving her lungs necessary time to heal. That machine, known as ECMO, or extracorporeal membrane oxygenation, saved her life.
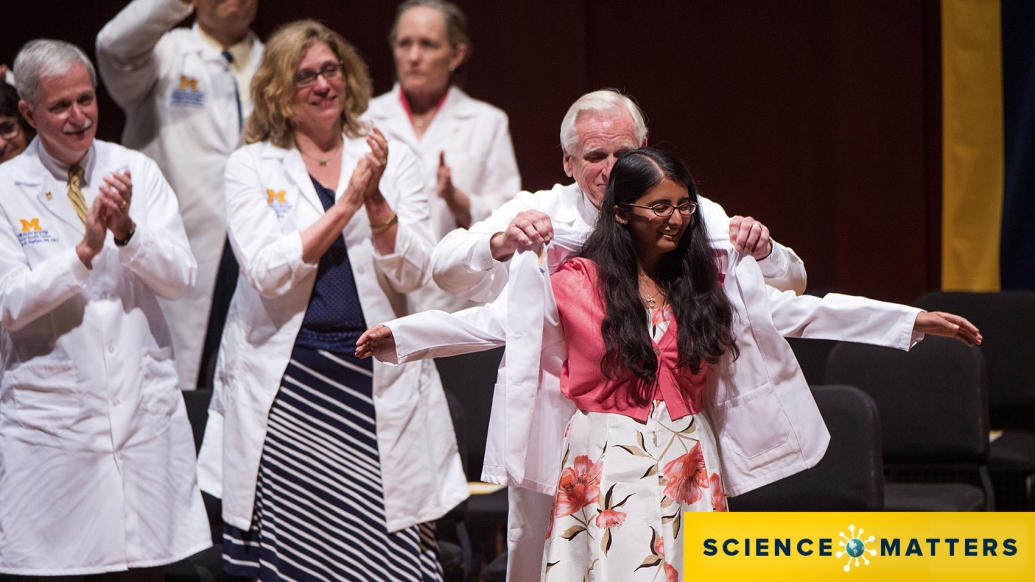
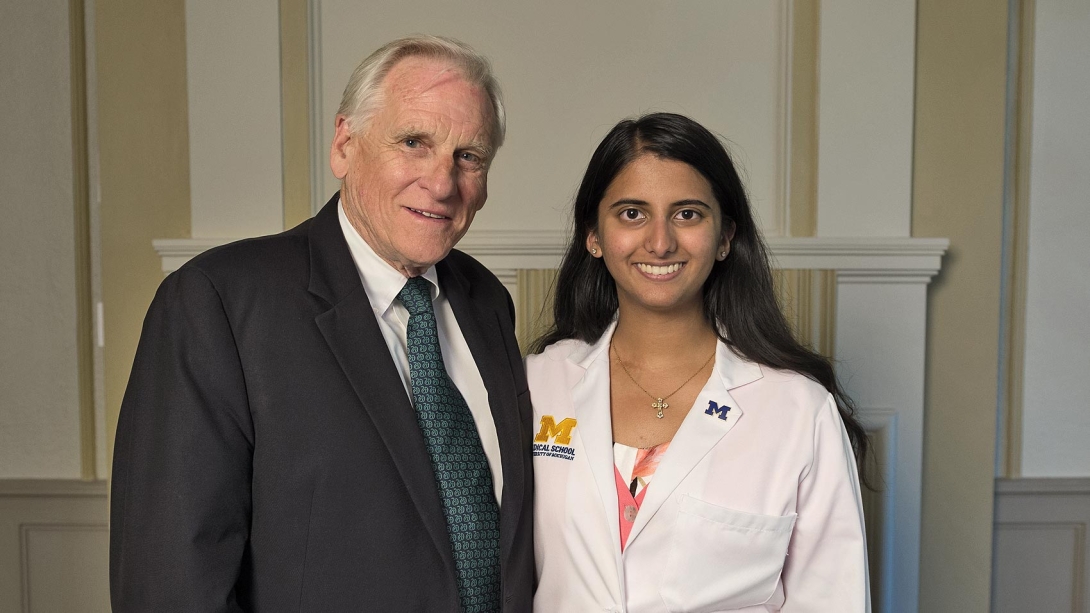
Twenty-one years later, Cheriyan was at U-M again — this time walking the stage in the 2015 White Coat Ceremony, a ritual welcoming students into medical school. And Robert Bartlett, M.D., the Michigan doctor who devoted his career to developing ECMO, "cloaked" Cheriyan with her first official white coat.
"I felt like I had come full circle from the Mott NICU to Michigan Medical School," she says. "It was such a special experience to share that moment with Dr. Bartlett and for him to join me in the beginning of my own journey as a physician. His work is the reason I'm here today."
Bartlett says he's proud to see how far she's come.
"There wasn't a dry eye in the house," he says of the ceremony. "That was a very emotional time, as you might imagine."
Funding for a 'far-fetched project'
It took Bartlett and his colleagues more than a decade of persistent research before the lifesaving innovation reached patients such as Cheriyan.
"At the time, it wasn't just an out-of-the-box idea. It was an outrageous one," says Bartlett, professor emeritus of surgery at Michigan Medicine and the "father of ECMO." "In the beginning, most neonatologists thought this was a pretty crazy, far-fetched project."
Bartlett and colleagues started the journey to pioneer ECMO in the 1960s. It was the early days of pediatric heart surgery, and the mortality rate for children was 50 percent, many dying within days of their procedure. Doctors knew patients could survive if they had a few more days to recover.
The heart-lung machine made cardiac surgery possible, but it caused lethal blood damage when used for more than an hour. These early "artificial lungs" delivered oxygen directly into the blood, which turned out to be harmful after a short time.
Bartlett and colleagues set out to create a gentler oxygen delivery system with fewer side effects. Research teams developed membranes to prevent oxygen from contacting the blood directly — the secret to extending the use of heart-lung machines. Using membranes for oxygen and CO2 transfer allowed the use of modified heart-lung machines for days. The new machine and technology was called ECMO.
Bartlett and other researchers wondered if ECMO could be used for life support during severe heart or lung failure.
In 1975, Bartlett reported the first neonatal survivor of ECMO, a baby battling such severe lung damage that ECMO was used as a last-ditch effort to save her life. After seven days on ECMO, she recovered.
"Our wild idea worked," Bartlett says. "And it has continued to work remarkably well in all types of patients with heart or lung failure."
But it took years of dogged research and animal and clinical trials — backed by millions of dollars in federal funding from the National Institutes of Health.
And today, ECMO has saved tens of thousands of patients around the world, including 2,500 at the University of Michigan, according to the Ann Arbor-based nonprofit Extracorporeal Life Support Organization.
Paying it forward
As for Cheriyan, now 23, she stumbled upon Bartlett's name while studying biomedical engineering as an undergrad. She sent him an email reading, "Thank you for saving my life."
SEE ALSO: Twin Sisters Survive a Lethal Bond, then Laser Surgery, in the Womb
She went on to spend four years as a research assistant in his lab.
"It's a huge privilege to be a part of such an impactful project and being able to give back to the research that made such a difference in my own life," she says. "I want to pay it forward."
Tani Shtull-Leber, who will graduate from U-M Medical School in May and is preparing for an emergency medicine residency in Phoenix, also found his way from the NICU to Bartlett's lab.
At birth, Shtull-Leber experienced lung failure, turning blue and unable to breathe. He was put on ECMO at a St. Louis hospital near his home at the time.
"My lungs needed more time to develop, and ECMO bought me that time," he says. "I would not have lived past two days without ECMO."
Decades later, Shtull-Leber ended up in U-M Medical School — the same institution where his father, Steven Leber, M.D., is a pediatric neurologist. And Shtull-Leber also ended up working with Bartlett in the ECMO lab.
"It was really inspiring to see how Dr. Bartlett and everyone in his lab continue to push the boundaries to extend life," he says.
"We would not be able to advance the field without federal NIH funding to support ideas that may sound 'out there,'" Shtull-Leber adds. "It's important to support research even when it's hard to see if there's going to be a payoff. It's so hard to predict when the next big breakthrough or innovation is going to be. ECMO is an example of that."
Advancing ECMO
Today, researchers in Bartlett's ECMO lab remain steadfastly committed to work in the field.
Projects include using ECMO for an artificial placenta to tackle extreme prematurity, work to optimize implantable artificial lungs and to extend the life of organs before a transplant.
All ideas the medical industry won't invest in until research has proved they work, which is why federal funding is critical to discovery, Bartlett notes.
"What may seem like a pretty wild idea can someday be a critical treatment," he says.
"It's extremely satisfying to see how far ECMO has come. We periodically hear from families who benefited and heard we had something to do with it. It's a great feeling, but also as scientists, this is what we do. It's what we are supposed to do."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





