Most people aren’t familiar with the second most common form of dementia. What all patients and caregivers should know.
6:00 AM
Author |

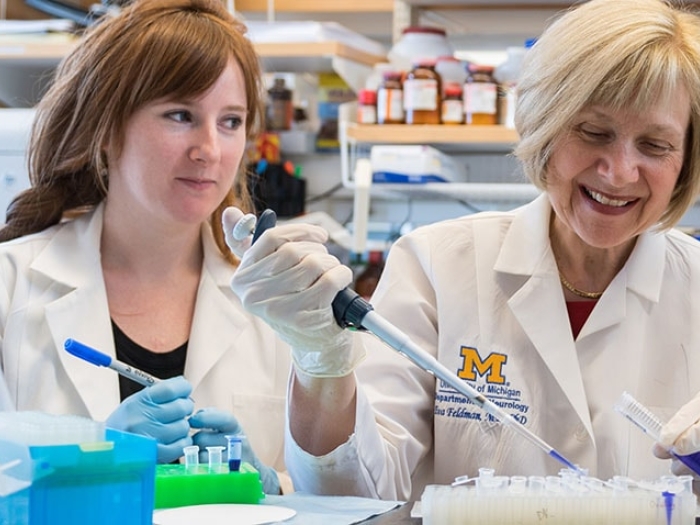
When I accepted an internship with the Michigan Alzheimer's Disease Center, I had a basic understanding of dementia. I knew it was a growing problem for older adults.
But I did not realize its complexity, nor how much there was to learn about dementia in all its forms.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Throughout my three years at the center, in a variety of positions, I gained exposure to not only the medical and research side of dementia but also the education, caregiving and support side. Of all of my roles and responsibilities at U-M, the most memorable and meaningful was my role as a Lewy body dementia support group facilitator.
This role made me a passionate advocate on behalf of those with Lewy body dementia and their families. With the caregivers' experiences in mind, this is what I wish all people knew about Lewy body dementia.
Lewy body dementia is an umbrella term.
It refers to both Parkinson's disease dementia or dementia with Lewy bodies.
Lewy bodies are made of alpha-synuclein, a protein found in the brain that plays a role in communication between brain cells. With all forms of Lewy body dementia, the alpha-synuclein clumps inside neurons and causes them to slowly die.
Symptoms and diagnosis depend on where in the brain the protein clumps form and damage cells. For example, if Lewy bodies first form in the cerebral cortex, one will have a loss of function in information processing, perception, thought and language, and will most likely be diagnosed with dementia with Lewy bodies, as cognition has been affected first.
If Lewy bodies first form in the midbrain, movement will be affected first, leading to a diagnosis of Parkinson's disease. If Lewy bodies then accumulate on regions of the brain that affect cognition, one will then be diagnosed with Parkinson's disease dementia.
Lewy body dementia is common but not well-known.
Lewy body dementia is the second most common type of dementia in the United States, affecting an estimated 1.4 million people. It is not a new disease, yet it is frequently unheard of, even in the medical field. Now that imaging and cognitive testing have improved, clinicians are able to diagnose Lewy body dementia sooner in its progression.
SEE ALSO: What to Do When a Loved One with Lewy Body Dementia is Hospitalized
An earlier diagnosis means more individuals will be living longer with knowledge of the disease, leading to an increased need for services and resources.
Lewy body dementia is often initially misdiagnosed as another type of dementia.
Diagnosing Lewy body dementia is not always easy and cannot be certain until a postmortem autopsy has been completed. Neurologists have no easy way of looking inside the brain to give patients a concrete diagnosis, but they instead diagnose based off neurological exams that are often supplemented with brain imaging or biomarker tests.
Since the initial symptoms of Lewy body dementia are similar to those of Alzheimer's disease or Parkinson's disease, individuals will often be initially misdiagnosed or not diagnosed until later in their disease.
What works for Alzheimer's may not work for Lewy body dementia.
Since Lewy body dementia affects motor function, sleep and behavior as well as cognition, caregivers are faced with specific challenges that differ from other dementias. Attending an Alzheimer's disease support group may be helpful, but it may not cover the range of symptoms or situations a Lewy body dementia support group will cover.
And certain medications, such as haloperidol, are often prescribed to Alzheimer's patients with disruptive behavior but can have severe side effects in someone with Lewy body dementia.
Hallucinations are common but not always frightening.
A hallucination is an experience with the perception of something that is not actually there, whether that be hearing, seeing, smelling or feeling. Generally, one is aware they are hallucinating.
Most commonly with Lewy body dementia, individuals will have visual hallucinations of small people, children or animals. Oftentimes these hallucinations are not threatening and do not need to be treated with medication.
Try to see the positives, and be mindful.
Caregivers often say that there are ups and downs and some hours, days or weeks may be much better than others.
SEE ALSO: My Lewy Body Dementia Journey with the Love of My Life
But seeing caregivers just once a month, I noticed positive personality changes. Caregivers become more patient, calmer and more focused on living in the moment. While nobody wants to watch their loved one decline or to become a caregiver, there is wisdom to be gained from this life experience that others will never know. Reflection and mindfulness can help to improve the quality of life not only for the caregivers, but for their loved ones as well.
Lewy body dementia is a dance.
A caregiver once referred to her experiences with Lewy body dementia as a dance: learning to accept it as a part of life, working through the highs and lows, navigating new medications and symptoms, trying to find joy in the moments, never quite knowing what the next step will be but feeling free to flow with it.
Visit the Michigan Alzheimer's Disease Center for more resources and for information on Lewy body dementia support groups.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!