Using their knowledge of the musculoskeletal system, physiatrists are playing a greater role in cancer care.
1:00 PM
Author |

Cancer patients are sometimes bewildered by the number of medical professionals who become part of their treatment team.
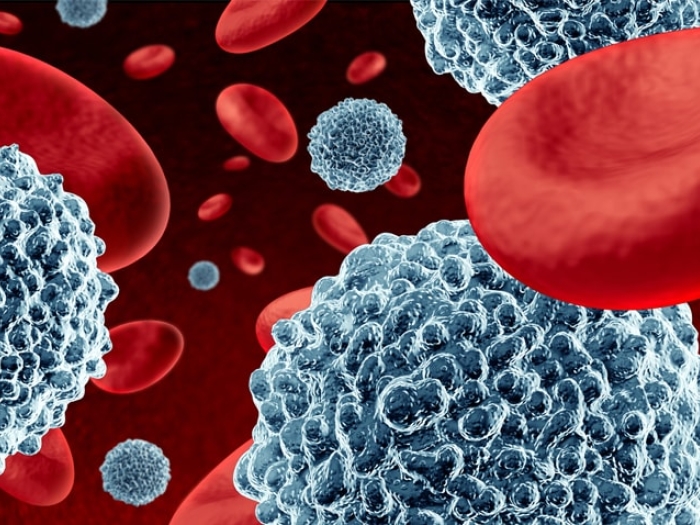
SEE ALSO: How Very Aggressive Cancer Cells Use Energy to Grow
A growing number of cancer centers are adding yet another clinician to the mix: the physiatrist.
Physiatrists, who are doctors with training in physical medicine and rehabilitation (PM&R), are increasingly found in the field of cancer symptom management and recovery.
That's because their training allows them to focus on the effects that cancer has on nerves, muscles, bones, joints and the brain.
"We're often able to zero in on impairments and subtle changes in mobility that others on the oncology team might not see," says Sean Smith, M.D., director of cancer rehabilitation at the University of Michigan Rogel Cancer Center.
It's important, then, that physiatrists become a part of a patient's multidisciplinary cancer care as early as possible, rather than after a marked decline in function.
Smith recently answered some questions about his work.
Why are physiatrists a vital part of cancer care?
Smith: Managing pain is a key focus for many patients. We prescribe and manage pain medications, joint injections and nerve blocks, and work with the oncology team to help limit the toxicity and symptom burden of chemotherapy.
We help patients at risk for falls; those with neurogenic bowel or bladder dysfunction; and anyone facing challenges to living independently. We screen patients during and following treatment for physical and cognitive impairments and advise them on strategies to maintain or increase function. We can provide home-based exercises to improve not only physical function but also mood.
When mobility is an issue, we are there to recommend the right equipment — everything from splits and braces to orthotics, walkers and wheelchairs. Physiatry can play an important role in preparing patients to return to daily living.
What are some of the most common cancers you encounter?
Smith: One of the most common diagnoses I see is breast cancer. That's partially due to the sheer volume and long survival of these patients, many of whom suffer from neuropathy. Head and neck cancer patients are also frequently referred for our services; many of their symptoms are highly receptive to the types of treatments we provide, such as nerve blocks and Botox injections to relieve pain.
SEE ALSO: What Cancer Patients Should Know About Nutrition
While sarcoma is far rarer than either of these cancer types, due to the musculoskeletal aspects of the disease, I frequently see these patients and attend the sarcoma tumor board as often as possible.
Is the growth of PM&R in oncology a national trend?
Smith: It is, and Michigan is playing a leading role. For example, in its most recent care guidelines, the American College of Surgeons' Commission on Cancer places more emphasis on patient-centered services like those we offer. The American Cancer Society also recognizes the need for rehabilitation services to identify and treat specific impairments to physical, cognitive and psychosocial functioning.
And the American Society of Clinical Oncology's member blog, The ASCO Post, regularly publishes a column that I edit called "Physiatry in Oncology Care." All of these signs point to recognition that cancer centers are taking a more active role in maximizing patients' quality of life after treatment.
How does cancer rehabilitation work at U-M?
Smith: I launched the program more than two years ago, and our cancer services are definitely growing. Today, we see patients in multiple locations. Many of the patients we see are referred to the Symptom Management and Support Care Clinic at the Rogel Cancer Center. Bone marrow transplant patients who experience nerve and musculoskeletal issues are seen on-site in the hospital. I also see patients off-site within the PM&R clinic in the Burlington Office Center in Ann Arbor.
What do you find most rewarding about your job?
Smith: The best part of my job is working with cancer patients — they're a very special group. They're so eager for information and reassurance, and they tend to be much more invested in their own care. Cancer patients are good at seeing the big picture; they have a wise perspective on life. I learn from them and am inspired by them every day.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!