As their 16-month-old fourth child undergoes treatment for a complex heart condition, two parents find ways to help others on similar journeys.
7:00 AM
Author |

With three happy, healthy kids at home, Gail and David Schupbach had no reason to expect any surprises when they went in for their 24-week ultrasound for Baby No. 4.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
That all changed when their ultrasound tech saw something abnormal.
"Honestly, we weren't that scared at first," says Gail. "We were told we'd learn more when we saw a specialist, and we hoped maybe it was even a false positive."
They were referred to a University of Michigan C.S. Mott Children's Hospital pediatric cardiologist who sees patients at their local hospital in Lansing, Michigan.
Monica Goble, M.D., determined that the baby did have a combination of congenital heart defects (CHDs), including a complex form of pulmonary atresia, with tetralogy of Fallot.
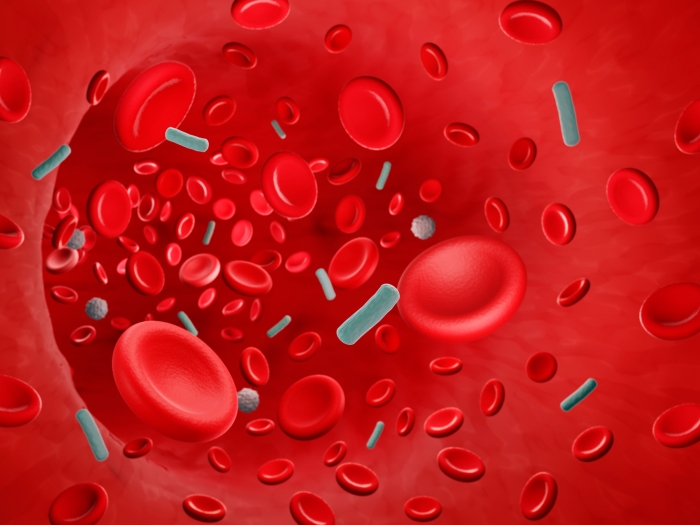
"Essentially, the pathways from the heart to the lungs didn't form correctly, affecting the way the blood flows through the heart and lungs and on to the body," Goble says.
The Schupbachs were sent to the Congenital Heart Center at C.S. Mott Children's Hospital in Ann Arbor for additional testing.
"We felt very comfortable with the team there. We knew we were in good hands, and our plan was actually to have the baby there so she'd have access to the full heart team right away," Gail says.
Three months later, little Ruby had other plans.
Ruby's arrival
Shortly after midnight on a Friday in October, at 38 weeks and three days pregnant, Gail went into labor.
"We could tell things could happen quickly, so we decided to just make the 10-minute drive to our local hospital," she says.
The Schupbachs spoke with Goble by phone in the wee hours of the morning, and she assured them they were in good hands. When Ruby was born that day, Goble was the first pediatric physician in line to see her.
Aside from being a bit early, Ruby was doing well. She spent a few days under observation in the neonatal intensive care unit before being transferred to Mott.
Over the next week, Ruby underwent a battery of tests to further study the structure of her heart, blood flow and oxygen levels. She was discharged to give her time to grow, under the close supervision of Goble, who saw the Schupbachs in her Lansing office weekly.
A month later, in late November, Ruby came back to the hospital for her first operation to place a shunt, a connection between blood vessels to improve blood flow from her heart to her lungs.
An additional operation in March allowed doctors to place another shunt. During that procedure, Ruby's surgeon, Jennifer Romano, M.D., started preparing the path from Ruby's heart to her lungs for a future procedure to create more established heart and lung circulation.
"We try to give babies like Ruby time to grow as much as they can before their first repair operation," Romano says. "We want to allow her pulmonary arteries to grow and develop so we can create 'normal' blood flow when it is time for surgery."
In the meantime, Romano, Goble and interventional cardiologist Jeff Zampi, M.D., kept a close eye on Ruby, performing a few catheter-based procedures along the way to maintain blood flow until the time was right.
The team anticipated that Ruby would be ready for her repair procedure to establish a more normal circulation pattern between the heart, lungs and body in the fall of 2017.
Once again, though, Ruby had her own plan.
"We went in for a diagnostic catheter procedure with Dr. Zampi, and they found she was actually already ready for her repair," says Gail. "We're excited about what it means for Ruby. … We are so pleased she's growing well enough to be ready for the operation, but most of all we're excited that she'll be able to have a 'normal' childhood for a while."
You feel very alone when you hear your baby will be born with a heart defect. You have a hundred questions, and it's all you can think about, but you also feel like no one else has been down the same road.Gail Schupbach
Overcoming isolation
"Normal" seemed out of reach for the Schupbachs at one point.
"You feel very alone when you hear your baby will be born with a heart defect," says Gail. "You have a hundred questions, and it's all you can think about, but you also feel like no one else has been down the same road."
SEE ALSO: Fixing a Tiny Heart: Open Heart Surgery at 4 Months Old
Gail recalls a physician checking on her when Ruby was in the hospital.
"I was crying, again. I cried a lot during the early consultations. She recommended I talk to parents who had gone through similar journeys, and the nurses made some suggestions of other moms to connect with. It was so good to see that the concerns I was feeling were not unusual. Having people to connect with finally changed everything."
That's why the Schupbachs have made promoting awareness of CHDs a part of their family mission.
"Whatever we can do to share our story so other newly diagnosed CHD families won't feel so alone, to help them know how common this is and how good their child's prospects can be, and to know that this doesn't have to define them. We're committed to doing all we can," Gail says.
David, who works as the digital outreach coordinator for the Michigan Senate, worked with legislators on an official proclamation for Congenital Heart Defect Awareness Week for 2016 and 2017. (This year it falls on Feb. 7-14.)
Gail is the coordinator for a Pediatric Congenital Heart Association mid-Michigan parent group, where she works to build a stronger network for CHD families in mid-Michigan with an eye on increasing statewide advocacy efforts.

Ruby's outlook
While Ruby's heart will never be normal and she may require future procedures in addition to lifelong monitoring, surgery should allow her circulation to function well, despite the structural differences.
In the meantime, little Ruby continues to thrive at 16 months old. The family is preparing for her open-heart surgery this month.
"She saw a developmental specialist with the Congenital Heart Center this fall," says Gail, proudly. "She's completely on track developmentally, and we're looking forward to a month or so from now, after recovery, when she'll have the opportunity to just be a little girl!"

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!