Your guide to that and other frequently asked questions about the most common sexually transmitted infection in the United States.
11:41 AM
Author |
Answer #1: HPV is a sneaky little virus. Most people will get an HPV infection, but unless you specifically look for it, you probably won't notice it: It can produce warts but no symptoms. While most HPV infections go away by themselves, those that don't can sometimes cause cancers that develop over several decades.
If you've never heard of HPV, you probably have a lot of questions. Luckily, the experts at Michigan Medicine have answers. Read on to learn more about the virus, what problems it can cause and how best to prevent HPV infections.
What is HPV?
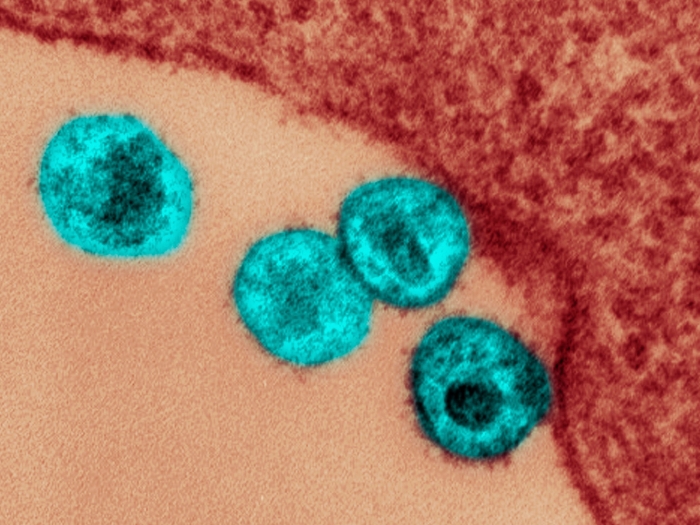
HPV, or human papillomavirus, is a virus that can only live in skin cells. There are more than 100 different types.
How do you get HPV?
HPV is transmitted when skin rubs against other infected skin. This occurs most often during sex, but there are lots of other ways skin-to-skin contact can occur.
What problems can it cause?
Some types of HPV, known as low-risk types, can cause warts. Depending on the HPV type, the warts will grow on dry skin, like that on your fingers and toes, or soft, wet skin that's found in places like the inside of your mouth, your genitals or your anus. You should talk to your doctor about how to remove these warts, but you don't have to worry about these HPV infections causing cancer.
Other, high-risk types of HPV can lead to cancer. Many people associate HPV with cervical cancer, but you can also get cancer from HPV:
-
in your vagina
-
on your penis
-
on your vulva
-
in your anus
-
in your throat, your tonsils, or the back of your tongue, which is known as oropharyngeal cancer.
How can you tell if you're going to get cancer from an HPV infection?
The short answer: Currently, you can't, although technology is in the works to better predict that.
The longer answer: Most people's immune systems clear HPV out of their bodies within one to three years. But if the virus lingers for a long time, it can become a part of your DNA, and then potentially cause cancer several decades later. (HPV can find its way into almost every chromosome.) Essentially, HPV doesn't want to cause cancer, but if you leave it alone long enough, it might.
Is the risk of getting HPV the same for everyone?
Yes. Whether it's even possible for you to get some cancers caused by HPV depends on your genitalia; you can't get penile cancer if you don't have a penis or cervical cancer if you don't have a cervix. Oropharyngeal cancer associated with HPV is far more common in men than women.
Is there anything I can do to prevent HPV infection and cancers caused by HPV?
Yes. You can get the HPV vaccine and undergo cancer screening (see "Are there any screenings for cancers caused by HPV?").
When should I get the HPV vaccine?
The optimal time is between nine and 12 years old. If you get it after you're 15, you'll need three doses instead of two doses within a year. The CDC recommends the vaccine up until age 26 and encourages you to talk to your doctor about getting it if you are between 27 and 45 years old.
SEE ALSO: Make Sure Your Teen Has Had These 4 Lifesaving Vaccines
Are there any side effects?
Sometimes the arm in which you got your shot will be red, sore or swollen afterward. You might get nauseous, dizzy or tired; you could develop a fever or a headache. There might be some muscle or joint pain. Children are more likely to faint after receiving the vaccine. However, all of these symptoms are typically mild and pass quickly. Other rare side effects have been reported.
Will the HPV vaccine help me fight off HPV if I've already been infected with the virus?
Sort of. Once HPV enters a cell, it creates copies of itself that can re-infect you. The HPV vaccine makes antibodies that keep those new viruses from entering your other cells. For the cells already infected with HPV, you'll have to rely on your immune system to clear out the virus, which usually takes between one and three years.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Are there any screenings for cancers caused by HPV?
For cervical cancer, yes. Generally, women should have these done every three to five years up until age 65 and more frequently if they test positive for HPV or if pre-cancerous or cancerous cells are found during one of their exams.
Screenings for anal cancer are also available but not widely done. If you're having anal sex, you could ask your doctor whether this screening would be worth pursuing.
For all other cancers caused by HPV, not at the moment. That's why vaccination is so important.
Does health insurance cover the HPV vaccine?
It should if you're under age 27. But double-check with your specific plan to make sure.
What if I'm older or I don't have health insurance?
You could pay the out-of-pocket cost, which is $140.59 per dose for adults and $196.32 per dose for children.
A variety of options could also help reduce the cost of the vaccine. For instance, Merck, the maker of the Gardasil 9 vaccine (the only HPV vaccine available in the United States), offers a patient assistance program. And the Vaccines for Children Program is a partnership between the CDC, local health departments, and doctor's offices to distribute free vaccines, including the HPV vaccine. University health clinics and Planned Parenthood can also provide low-cost alternatives.
In some other countries, you can get Cervarix, an HPV vaccine that provides similar protection to Gardasil 9 against cervical cancer.
Where can I get the HPV vaccine?
Pediatricians, family medicine providers, OBGYNs, pharmacies. You can ask your doctor, health insurance representative or pharmacist where would be most convenient and cost-effective for you.
Diane M. Harper, M.D., M.P.H MS, and Michelle M. Chen, M.D., served as the experts for this guide.
Like Podcasts? Add the Michigan Medicine News Break on iTunes, Google Podcast or anywhere you listen to podcasts.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!