Patients who receive an implanted mechanical pump to support heart function must follow certain lifestyle guidelines. A nurse explains the basics.
1:00 PM
Author |
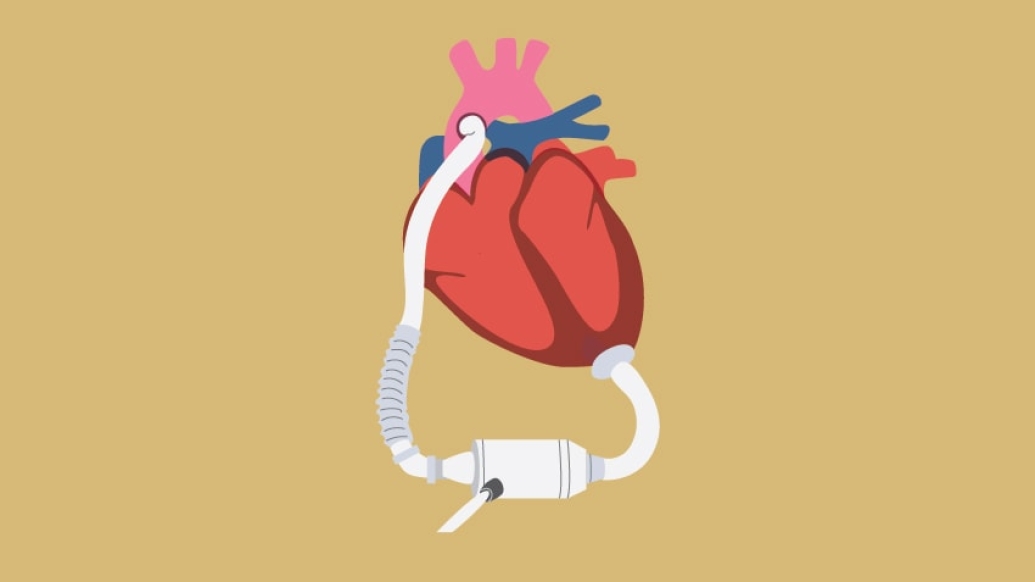
A ventricular assist device, or VAD, is an implantable pump that helps a weak heart circulate blood to the rest of the body.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Patients with advanced stages of heart failure are often treated with a VAD, which can be used as a bridge while awaiting a heart transplant.
For those who are not suitable transplant candidates, the pump can provide long-term support — treatment known as destination therapy.
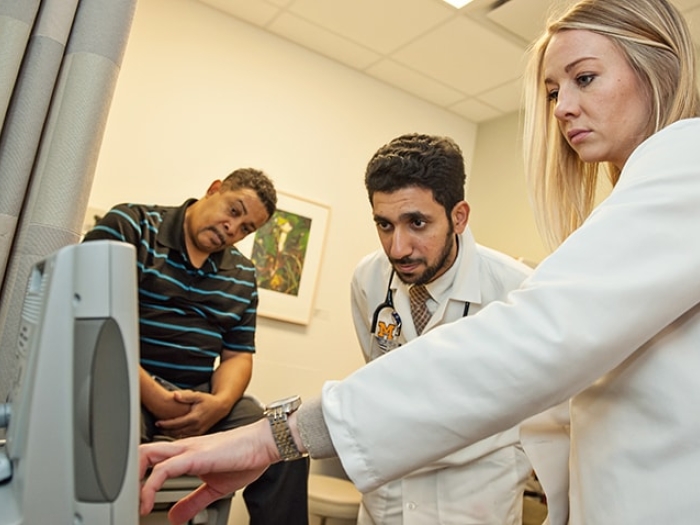
Rena Lucier, R.N., who works with VAD patients at the University of Michigan Frankel Cardiovascular Center, knows that recipients often have many questions.
That's why she and her colleagues are here to help.
"Our VAD team is committed to making sure patients understand everything involved with a VAD and are able to leave the hospital with confidence," says Lucier, who shared answers, in her own words, to some of the most common queries she receives:
How do I learn to operate a VAD?
At the Frankel CVC, we educate patients and their caregivers about every aspect of their VAD, including how it operates, how to change the batteries, what the alarms indicate, how to troubleshoot and the importance of keeping the abdominal area where the driveline (a cable that connects the pump to its controller) exits the body clean.
SEE ALSO: For Patient Awaiting New Heart, a Ventricular Assist Device Brings Hope
In fact, a patient cannot leave the hospital until they have a full understanding of their VAD and can manage it with confidence. We even have outings, both supervised and unsupervised, where the patient and caregiver take a trip outside of the hospital setting prior to discharge to make sure they feel confident.
Can I shower with a VAD?
Patients cannot shower until the site where the driveline exits the body is fully healed, which can be anywhere from three to six months or longer. The time varies with each patient.
Can I drive with a VAD?
Patients implanted with a VAD cannot drive during the first three months following hospital discharge. After this time, the VAD cardiologist will re-evaluate a patient's ability, from a medical standpoint, to drive. It is important that a patient has recovered from the surgery and does not have any VAD-related issues or ongoing medical concerns. Patient safety is our overall concern.
When can I be left alone?
A VAD patient must be with a trained caregiver for at least three months following surgery. If a patient doesn't have an available caregiver, we help them explore options such as family, friends, neighbors or church members. It's important for a patient to have a caregiver nearby at all times. This is re-evaluated after three months to determine if a patient can be alone.
Do I need to follow a special diet?
We recommend a low-sodium diet to prevent fluid retention. Most of our patients are accustomed to this type of diet. Also, because the VAD patient is on the blood thinner warfarin — which reacts with vitamin K found in such things as leafy vegetables and lettuces — diet is important.
Can I travel with my VAD?
Once a patient has recovered from surgery and is strong enough, travel is permitted. Patients must know the locations of nearby VAD centers in case of an emergency.
The Frankel Cardiovascular Center's VAD team locates the hospitals that are equipped to care for VAD patients along their travel route and at their destination. We provide VAD hospital contact information to the patient, and we notify these hospitals that our patient is traveling in their area in case the patient contacts them and requires assistance.
What about exercise?
We encourage patients to be active. Patients must avoid contact sports and swimming (the device is mechanical, so it cannot get wet). We want our patients to get back to what they enjoy doing, within reason. We also refer our patients to cardiac rehab, which helps them get back into an exercise program.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!