Synthetic material used to help treat a common condition has been linked to problems and lawsuits. A Michigan Medicine board-certified urogynecologist explains the issues.
1:00 PM
Author |
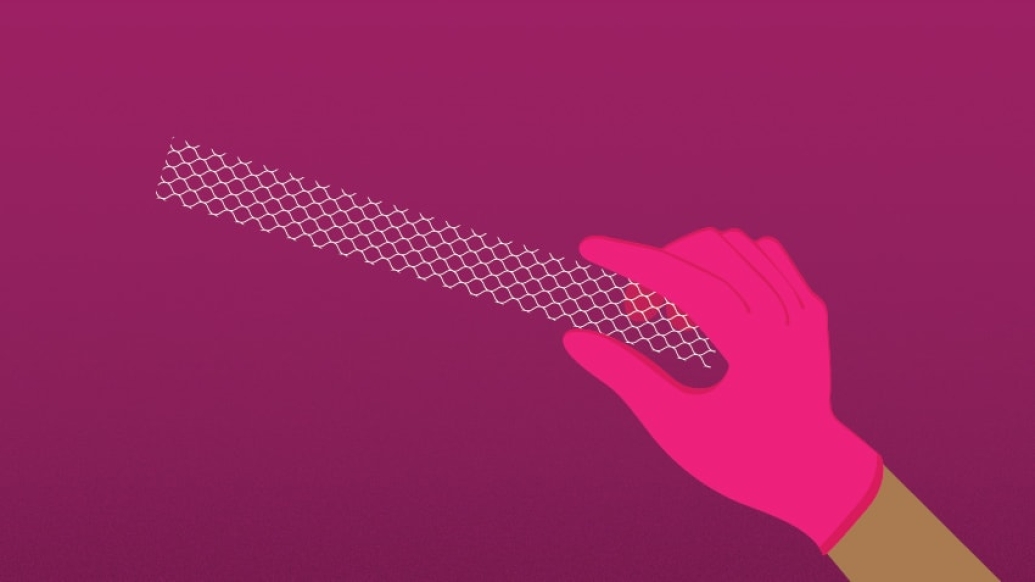
Questions surrounding pelvic mesh could leave some women feeling trapped.
Mesh material, used to treat pelvic organ prolapse and stress urinary incontinence, was marketed by its manufacturers as a durable surgical method for repairing these challenging problems compared to other corrective surgeries with a high failure rate.
ASK ALEXA: Add the Michigan Medicine News Break to Your Flash Briefing
But pelvic mesh has faced increased scrutiny from the U.S. Food and Drug Administration due to reports of frequent postoperative complications. Thousands of patient lawsuits have been filed citing mesh-related pain, bleeding and infection, among other problems.
Women should be informed but not necessarily fearful, says Megan Schimpf, M.D., an associate professor of obstetrics and gynecology and urology at the University of Michigan.
"We don't want to get the message out there that all mesh is bad, or that mesh has to be removed simply because other women are having problems," Schimpf says, noting that some problems with mesh surgery may be related to how it was placed or surgeons lacking training or experience.
"Many women are happy and symptom-free after mesh surgery."
It's also important, she notes, for patients to understand that there are different kinds of mesh surgery — and each one has varied risks and success rates.
Mesh implanted to fix urinary incontinence, which occurs when a woman coughs or sneezes, has a very high success rate with low risk of complications. It is regarded as the best surgery to fix this type of urine leakage and involves placing a small sling of mesh material underneath the urethra, which is the tube from the bladder to the outside.
Mesh can also be used to fix prolapse, or dropping of the pelvic organs, including the bladder, vaginal walls or uterus. This can be implanted either through the abdominal wall (including with laparoscopic, or robotic, surgery) or through the vaginal opening.
Prolapse surgeries where mesh is implanted through the vaginal opening have the highest risk of complications.
The American Urogynecologic Society issued a statement saying mesh for prolapse is appropriate for some patients, but more research and better credentialing is needed.
Not all surgery for prolapse includes mesh material. Other surgical and nonsurgical options are available.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Michigan Medicine surgeons have pioneered an approach to prolapse surgery that doesn't involve any abdominal incisions or mesh material. Dissolvable sutures are used to attach the top part of the vagina to a ligament deep in the buttocks. Patients having this procedure typically are able to go home the following morning with little pain.
"We can achieve excellent repair of prolapse without any mesh material at all, and therefore without taking on any of these risks," Schimpf says. "That's one of the things we're really proud of here at Michigan."
Still, given recent news stories, women who have already had mesh placed for prolapse or incontinence might be concerned or confused about their own risks and what steps to take. Some women may have been contacted by a lawyer about their mesh and are unsure how to respond.
Schimpf, who is also the chair of the public education committee for the American Urogynecologic Society, answered some common questions about the issue:
Questions about pelvic mesh
Is pelvic mesh safe?
Schimpf: I do think that it's safe when used in the right hands in the right patients.
Mesh is made out of a suture material that has been used widely in surgery and medicine for many years. That material is woven into a fabric that has been used in many procedures, including cardiothoracic surgery and hernia surgery.
Mesh surgery for stress urinary incontinence is often thought of as the gold standard or best surgical option for this problem. Risks are low, and my patients are so happy after this procedure. Many are out running marathons, playing with their grandkids and living their life again without leakage after that surgery.
Prolapse mesh is safe, too. Here at Michigan, we only place mesh through the abdominal wall, using our laparoscopic skills to do this without any major incisions. My patients after this surgery are also extremely happy. Some of them don't even feel like they've had surgery. We don't perform the vaginal mesh surgery that has caused more complications.
So, I don't think there's any inherent risk in having mesh placed, but there are specifics that a woman needs to know about what surgery she's having. As long as you truly have a problem — and have a surgeon well-versed in using it — mesh can help.
What women should consider surgery for prolapse or incontinence? Is it the only option?
Schimpf: If a woman notices that her prolapse symptoms or incontinence is starting to affect her lifestyle and activities she wants to do, it's time to see a urogynecologist to discuss in more detail. Your bladder or bulge shouldn't hold you back from enjoying exercise, your family, your hobbies or sex.
Some of these bothersome symptoms might include a vaginal bulge, pelvic pressure, or leakage of urine. See a urogynecologist if any of these things are happening.
Your appointment will include a discussion of your symptoms, an exam to assess for leakage or a bulge, and then a discussion of options. Surgery is one option, and in some cases, this might involve mesh material. Women should ask questions about other options besides surgery and whether there are multiple options for surgery.
What can go wrong?
Schimpf: We've learned a lot of about mesh in the past few years, which speaks to why having a surgeon with expert training and lots of experience is valuable.
For example, the mesh does shrink somewhat after it's put in the body. The surgeon needs to anticipate that and position it properly. If not, the mesh can tighten and pull on the muscles and pelvic floor. This can cause pain. These women can experience pain just when sitting still, when trying to exercise or when having sex. These tight muscles can also cause difficulties with urination or having bowel movements.
Mesh can also become exposed in the vagina. Women can feel it, or sometimes their partners notice something during sex. This can also cause bleeding or abnormal discharge.
Mesh can sometimes be positioned improperly, such as in the bladder or the bowels. If this happens, it needs to be removed surgically.
If I needed surgery for one of these problems, what kind of doctor should I see?
Schimpf: Seek out a surgeon who has specialized, formal training in urogynecology, which is called fellowship training. Then, ask your surgeon if they're board certified in female pelvic medicine and reconstructive surgery. The terminology can get confusing here; asking that person if they are trained and board certified in urogynecology is another way.
You can also ask that surgeon how many mesh procedures they've done each year. I would say that should be at least 20 to 25 annually for you to feel comfortable with their skill.
Any surgeon performing prolapse or incontinence surgery should be able to offer you the option to fix those problems with or without mesh material. Ask about those options and whether they are able to help you later if there's a complication — you want to see the doctors who can help you throughout anything that might happen.
If you need to have your mesh removed, the surgeon should have experience in that as well; ask if they've done that surgery before. The most informed surgeons also participate in national meetings so that they are up-to-date on new research and techniques.
I've already had gynecologic or pelvic mesh surgery. Should I be concerned?
Schimpf: If you're doing fine and you have no symptoms — if the surgery fixed whatever issue led you to have surgery — you should not worry. You do not need to have your mesh removed. Mesh doesn't expire. Even if the specific mesh product isn't on the market anymore, you don't have to have it removed.
SEE ALSO: Treating Postpartum Hernia: What New Mothers Should Know
If you're having pain, difficulty with intercourse, unexplained bleeding or discharge and you've had mesh surgery, see a urogynecologist and ask if it could be the mesh.
Depending on that expert's opinion, treatment of this can be complex. Because the mesh can cause muscle spasms and scar tissue, surgery is only part of the answer. We did a study here looking at patients who had their mesh taken out. Afterward, 50 percent still had some pain, though many women were improved.
We have other options, such as pelvic floor physical therapy, that can really help women who are still struggling after the mesh is removed.
A lawyer has randomly contacted me about my pelvic mesh. How do I respond?
Schimpf: Lawyers aren't a good way to get your medical care. Instead, contact the surgeon who put in your mesh in. Get a copy of your operative report and find out exactly what mesh product was used; they all have specific product names.
Be proactive to seek out your own medical care, not what lawyers are offering you. If you're concerned about trusting your original surgeon, you can also call the hospital where you had the surgery. They can get you the operative report and you can find a urogynecologist for a second opinion. Bring that report with you.
To schedule an appointment or learn more about the urogynecology program at University of Michigan Von Voigtlander Women's Hospital, call 734-763-6295 (Ann Arbor) or 248-305-4400 (Northville), or click here.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!