Better outcomes for infants with congenital heart disease mean U-M practitioners can now focus on early intervention to prevent developmental delays.
12:30 PM
Author |
For decades, survival was the only goal for babies undergoing heart surgery.
Not anymore.
"We expect a lot more now," says Karen Uzark, PNP, Ph.D., an outcomes researcher and nurse practitioner with the Neurodevelopmental Follow-Up Clinic at University of Michigan C.S. Mott Children's Hospital Congenital Heart Center.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
There has been a major shift in congenital heart disease treatment toward infants not just surviving, but thriving, she says.
"When you are worried about your baby making it through surgery, things like whether your baby is lifting his head up may seem less important at the time," Uzark says. "But we know now how well these babies can do, and so we want to make sure they have every opportunity to reach the same milestones as other babies."
In 2012, the American Heart Association published a scientific statement describing common developmental delays and disabilities in children with heart disease, emphasizing the need for screening and evaluation.
Developmental challenges
Babies who have cardiac surgery in their first year are more likely to have developmental challenges, ranging from delayed motor and language skills and feeding problems early in life to task organization challenges as they get older. With each, early identification is key.
Uzark and her colleagues have identified other risk factors, too. Babies who spent more than five days in the intensive care unit after surgery, for example, showed significantly lower scores in gross motor development at discharge than babies who spent less time in the ICU.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Their findings prompted Mott to introduce a multidisciplinary neurodevelopmental team that starts visiting any baby who is in the cardiovascular ICU for more than five days — collaborating with bedside nurses and parents to look for ways to prevent developmental delays. The team includes specialists in pediatric cardiology, physical therapy, occupational therapy, speech therapy, child life, rehabilitation and cardiac surgery.
"We work with the family on positioning their baby and other environmental things they can control, even in a hospital setting," Uzark says.
Many issues can be addressed through basic interventions, which is why programs like Mott's are so important.
He's climbing up stairs now and trying to run. Compared to another baby who hadn't had surgery, he's right where he should beMaria Hays
More tummy time
"We try to start the process early — even before surgery, when possible — to help parents understand some of the heightened risk their child will face and understand what they can do to help," Uzark says.
Some interventions are as simple as more tummy time. Conversations with parents revealed that they were worried about putting their babies on their tummies because of the incision on the chest.
"After a few weeks of no tummy time, any baby is going to resist being put on their tummy," Uzark says. "So we encourage families not to let much time go by without giving their baby time on their stomach to strengthen their muscles. When you reassure them ahead of time that even days after the procedure, the surgical site will be OK, that can go a long way towards helping families keep their baby on track."
Other tips include:
-
Avoiding overstimulation: The bright lights and busy sounds of an ICU can disturb a baby. The team suggests using white noise to minimize the beeps and hums, plus shades to create a sense of light during the day and dark during naps and at night.
-
Language: Data show that a parent's voice — even in an infant's first weeks — is a powerful foundation for language development, soothing and healing. The neurodevelopmental team encourages parents to read aloud to their babies, narrate their activities and even sing to them.
-
Movement: Children use their bodies to learn about the world around them. The team's physical and occupational therapists encourage parents to help babies bring their hands together and play games with their hands and feet, laying a foundation for them to reach and feed down the road.
-
Colors and patterns: The team ensures babies have access to positive visual stimulation like mobiles and mirrored toys, motivating babies to lift their heads to see the patterns on display.
The team also created a video available on the hospital's internal TV network to help parents understand and take some control of their child's neurodevelopmental growth.

Supporting parents
"It's not just about the baby — these parents go through so much. Sometimes something as simple as having a feeding tube in every baby picture can feel like defeat to a parent. It's like a reminder to them that their baby is sick," Uzark explains.
SEE ALSO: Ruby's Story: Normalizing Congenital Heart Defects for Michigan Families
She adds, "We try to identify ways to avoid oral aversions and prevent feeding problems from the start." Occupational therapists, for example, can give tips like dipping a pacifier in breast milk or formula during tube feedings to help babies associate sucking and taste with getting food in their tummies.
"Our focus is on reducing delays when we can and setting up the right interventions to get them caught up when delays are present," Uzark says.
Clinic follow-up visits
Families are encouraged to continue routine appointments at the Neurodevelopmental Follow-Up Clinic, an outpatient clinic whose multidisciplinary team is trained to identify delays and vulnerabilities early.
The clinic, led by pediatric cardiologist Caren Goldberg, M.D., M.S., and Jennifer Butcher, Ph.D., sees patients as young as 9 months old and then at regular intervals through their school years.
The clinic includes pediatric cardiologists, psychologists and neuropsychologists, a nurse practitioner, social worker and school liaison. Other specialists, including neurologists, feeding specialists, gastroenterologists and speech and occupational therapists, are available to collaborate as needed.
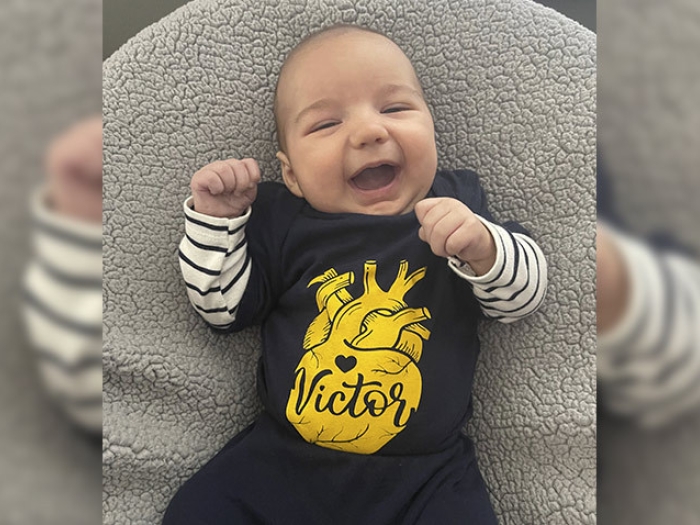
"For us, physical therapy was an important intervention," says Maria Hays, mom to 20-month-old Vincent. "The neurodevelopmental team arranged for Early On to come to the house and provide in-home therapy and help with things like feeding with a bottle and speech."
SEE ALSO: Newborn Screening Catches Baby's Critical Heart Condition
"If our work has shown us one thing, it's that long-term developmental impairments aren't a foregone conclusion," Uzark says. "There is a lot we can do and also a lot parents can do to help children with congenital heart disease during infancy."
And the power of information can't be overestimated.
"It was important for us to know where our baby was at with his development and know what we could do to help him," Hays says. "He's climbing up stairs now and trying to run. Compared to another baby who hadn't had surgery, he's right where he should be."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!